Today in 5-minute refresher lectures I will be discussing coeliac diseases. Always follow your local guidelines and seek specialist advice. This lecture is only intended as a brief overview.
VIDEO WILL BE ADDED SHORTLY
Coeliac disease is a systemic autoimmune disease primarily affecting the small intestine that occurs in people who are genetically predisposed.
Upon exposure to gluten, an abnormal immune response may lead to the production of several different autoantibodies that can affect a number of different organs.
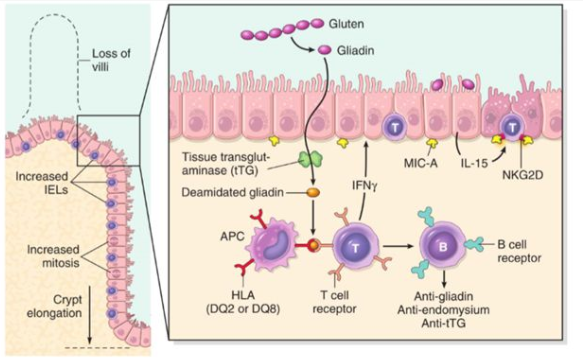

The genetics of coeliac disease is very complicated. The two main genes are HLA class II, HLA-DQA1 and HLA-DQB1. Different combinations alter the risk for developing CD. However, genome wide association studies has identified 39 non HLA loci that are associated with CD. The heritability of CD (proportion of the risk of CD attributed to genetic factors) is only 87%, Indicating there are environmental factors at play.
Megiorni F et al HLA-DQ and risk gradient for celiac disease. Hum Immunol. 2009;70:55–9
The prevalence of DQ2/DQ8 genes in the population is 1:3 and the likelihood of an effected person to develop CD 1:30. Since the DQ2 loci can be divided on two chromosomes or combined on a single chromosome, the inheritance pattern of CD can be both autosomal dominant or autosomal recessive.
Let’s say you have a patient in your practise with a family history of CD, what would be the likelihood the patient has CD themselves. (their HLA is not known yet). Their risk is 5-20% (Fasano et al 2003, Treem 2004).
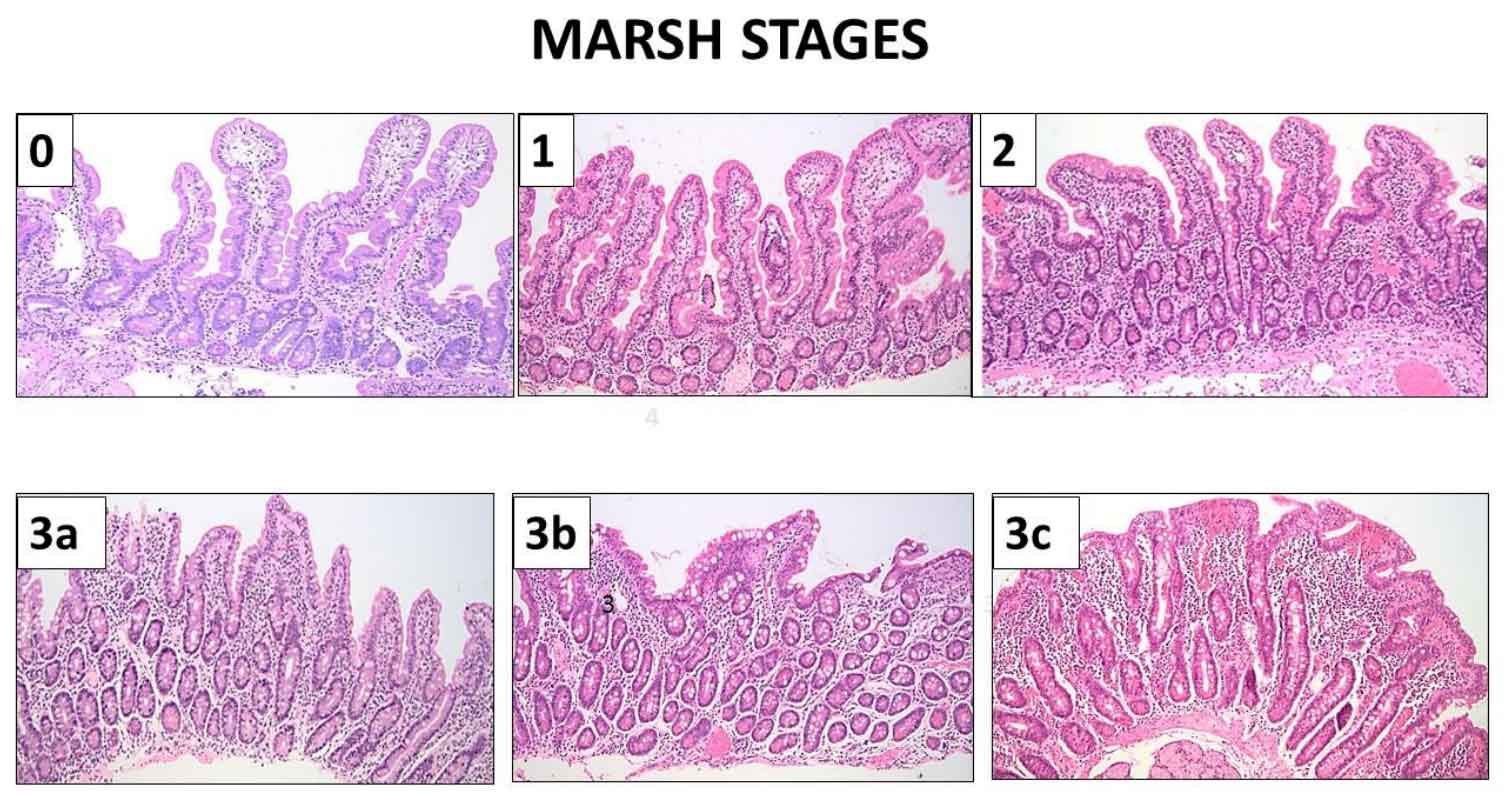
Genetic testing is useful for excluding CD, but with only a 1:30 penetrance does not prove CD. Most people with CD have positive coeliac serology with detectable auto-antibodies. Gastroscopy with duodenal biopsies is the “gold-standard” for diagnosis but is not always needed. For instance, if your patient has coeliac positive coeliac serology and symptoms resolve with excluding gluten. Often people with coeliac disease are unable to tolerate the daily gluten for 2 weeks and without gluten exposure the endoscopy will be normal.
Symptoms can include fatigue, depression, diarrhoea and abdominal pains. However almost all systems can be affected skin, cardiovascular, endocrine, neurological, metabolic, renal and rheumatological.
There is an increased cancer risk with coeliac disease. Therefore, it is important for patients to go on a strict gluten free diet even if the patient asymptomatic. A dietician review is very helpful. Compliance can be monitored with repeat coeliac serology after 6-12 months.